Fungal acne is often a misnomer for a condition known primarily as Malassezia folliculitis or Pityrosporum folliculitis, deriving its name from the yeast that causes it. This condition manifests in the skin’s hair follicles, leading to inflammation and breakouts that resemble bacterial acne.
However, unlike traditional acne, fungal acne is prompted by an overgrowth of this specific yeast, which thrives in warm, moist environments on the skin.
The breakouts associated with fungal acne tend to appear as uniform small pimples, commonly on the chest, back, and areas prone to excessive sweating. They can be accompanied by itching, a distinguishing factor from bacterial acne.
Since the treatment of fungal acne differs from other forms of acne, correctly identifying the condition is crucial for effective management.
Effective treatment targets the yeast with antifungal medications, and a healthcare provider can recommend various options suitable for the affected individual.
Furthermore, understanding preventative measures, such as maintaining skin hygiene and avoiding occlusive skin products, can help manage and reduce the risk of recurrence.
Understanding Fungal Acne
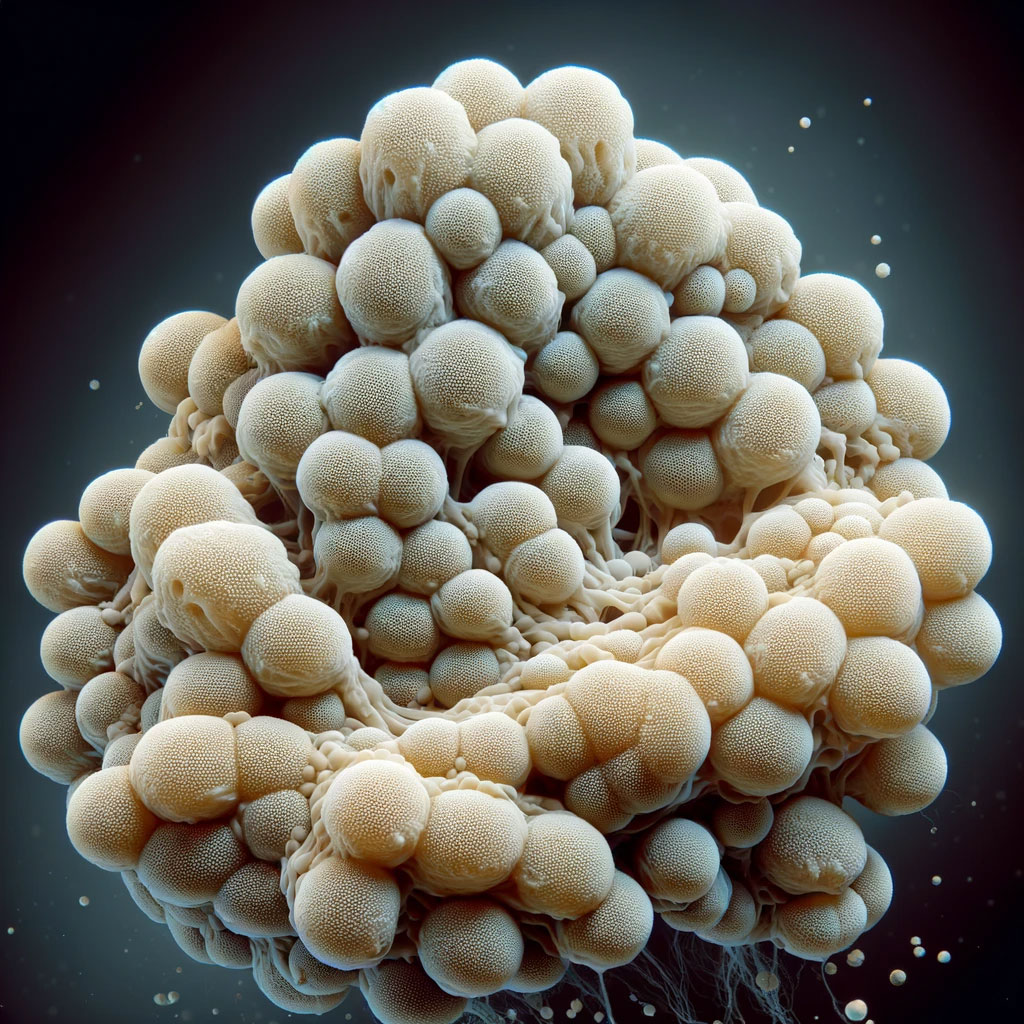
Fungal acne, a common misnomer, is not acne at all. It is a condition where yeast causes inflammation in hair follicles, leading to the development of itchy and uniform bumps on the skin.

Defining Fungal Acne
Fungal acne is a form of folliculitis, specifically caused by an overgrowth of Malassezia yeast. It is scientifically known as Malassezia folliculitis or Pityrosporum folliculitis. Unlike traditional acne, which is caused by bacteria and excess oil, fungal acne arises from a yeast overgrowth that thrives in moist environments.
Symptoms of Fungal Acne
Individuals with fungal acne typically experience clusters of small, itchy, red bumps (papules) and pustules across the skin. These bumps are often uniform in appearance and may become more prominent with sweating or in hot, humid conditions. Traditional acne treatments are usually ineffective against these symptoms because they do not address the fungal nature of the condition.
Fungal Acne Causes
The primary cause of fungal acne is the excess growth of Malassezia yeast within hair follicles. This yeast is normally present on the skin’s surface but can proliferate under certain conditions, such as high humidity, heat, and the presence of oils on the skin. Certain factors, such as immunosuppression, can also predispose individuals to develop an overgrowth of this yeast.
Differentiating Acne Types
When discussing acne, it’s crucial to understand that not all types are the same. The two that often get confused are fungal acne and bacterial acne, each with distinct causes and treatments. This distinction is vital for effective management.
Fungal Acne vs. Bacterial Acne
Fungal acne, medically known as Malassezia folliculitis or pityrosporum folliculitis, is usually due to an overgrowth of yeast – a type of fungus – within the hair follicles. This condition tends to present as uniform inflamed pustules which are often itchy.
Unlike traditional acne, fungal acne is not effectively treated with standard acne medications, and instead, requires antifungal treatments.
In contrast, bacterial acne, or acne vulgaris, is commonly caused by the bacteria Propionibacterium acnes. This type of acne is characterized by a variety of lesions including blackheads, whiteheads, and sometimes deeper cysts or nodules. Bacterial acne can exhibit a mixture of pustule sizes and levels of inflammation and typically does not cause itching.
Common Misconceptions
There’s often confusion when distinguishing between fungal and bacterial acne, as they can appear very similar. However, there are differences in appearance and symptoms between the two.
For instance, whiteheads and blackheads are typically associated with bacterial acne rather than fungal. Furthermore, fungal acne lesions tend to be uniform in size and more prevalent on the chest and back, while bacterial acne affects the face more diversely and can present lesions of varying sizes.

Affected Areas
Fungal acne, notably different from bacterial acne, targets the hair follicles, resulting in inflammation and breakout-like clusters. Primarily, it affects oil-rich regions where yeast can thrive.
Common Body Regions
Forehead (T-Zone): This is a prevalent spot for fungal acne due to its high oil production.
Chest and Back: Including the upper chest and upper back, these areas can develop clusters of itchy, small bumps.
Shoulders: Just like the back and chest, shoulders have higher concentrations of sebaceous glands, making them susceptible to fungal acne.
Upper Arms: Less commonly, the upper arms may also be affected, typically when there’s an overproduction of oil.
Risk Factors and Triggers
Understanding what contributes to the development of fungal acne can help in managing and preventing the condition. This section explores the factors that can increase the risk or trigger an outbreak.
Contributing Factors
Oil production: Excessive oil on the skin can create an ideal environment for yeast to thrive, leading to fungal acne. People with oily skin are more susceptible to developing this condition.

Heat and sweating: Warmth and moisture can encourage fungal growth. Those who live in hot climates or engage in activities that cause excessive sweating might experience more frequent outbreaks.
Weakened immune system: Individuals with a compromised immune system, such as those with HIV or taking immunosuppressive drugs like steroids, are at a higher risk of fungal acne.
Use of certain medications: Prolonged use of antibiotics can disrupt the natural balance of bacteria and yeast on the skin, possibly giving rise to fungal acne.
Underlying health conditions: People with diabetes often have higher glucose levels in their sweat, which can feed yeast. Thus, they may be more prone to fungal acne.
Hormonal changes: Fluctuations in hormones can increase oil production, potentially contributing to fungal acne.
Diagnosis of Fungal Acne
Diagnosing fungal acne requires specific approaches to differentiate it from other similar skin conditions like bacterial acne. The process typically involves a dermatological examination to observe the clinical signs and laboratory testing to identify the presence of yeast within the follicles.
Dermatological Examination
In a dermatological examination, a dermatologist looks for telltale signs of fungal acne, such as clusters of small, itchy red bumps commonly associated with folliculitis. They will closely inspect the skin, noting the distribution of the lesions, which often appear on the back, chest, and upper arms.
Unlike bacterial acne, which presents with comedones, fungal acne is characterized by uniform inflamed papules and pustules.
Laboratory Testing
To confirm the diagnosis, laboratory tests are necessary. Skin scrapings from the affected area may be examined under a microscope to detect the Malassezia yeast.
In some cases, a biopsy can be taken to provide a more definitive diagnosis. The collected sample is cultured to allow for the growth of the yeast, which helps in identifying the specific fungal organism responsible for the condition.
These laboratory results are critical as they ensure correct diagnosis and guide the subsequent course of treatment.
Treatment Options
When tackling fungal acne, it’s important to understand the different treatment options available. These options range from over-the-counter solutions and prescription medications to home remedies and adjustments to one’s lifestyle, each playing a crucial role in combating this particular skin condition.
Over-the-Counter Solutions
Over-the-counter treatments for fungal acne include antifungal creams and shampoos containing active ingredients like ketoconazole and selenium sulfide.
Products such as antifungal creams usually contain concentrations of ketoconazole ranging from 1% to 2%, which can be applied to the affected area. Shampoos containing selenium sulfide, like Selsun, are also recommended for their effectiveness against the fungi causing acne and can be used on the skin.
Prescription Medications
For more severe cases of fungal acne, healthcare providers may prescribe oral antifungal medications like itraconazole or fluconazole. These medications are potent in clearing fungal infections from the inside and are typically used for a short duration.
Topical treatments with higher concentrations of antifungal agents might also be part of the prescribed regimen, requiring careful adherence to the healthcare provider’s instructions to avoid any adverse reactions.

Home Remedies and Lifestyle
In addition to medical treatments, lifestyle changes can contribute to managing fungal acne.
Maintaining good hygiene, changing sweat-soaked clothes promptly, and using non-comedogenic skin products can help prevent the condition from worsening.
While some suggest home remedies like diluted tea tree oil for its antibacterial properties, it’s essential to consult with a dermatologist before applying any new substances to the skin, as they could potentially irritate or exacerbate the condition.
Prevention Strategies
Effective prevention of fungal acne centers on maintaining proper skincare and personal hygiene habits. By managing factors that contribute to yeast overgrowth, individuals can reduce the likelihood of developing this condition.
Skincare and Personal Hygiene
Skincare Routines: Utilize non-comedogenic and antifungal products to reduce the risk of yeast proliferation.
A dandruff shampoo containing ingredients like ketoconazole can be used on affected body parts due to its antifungal properties. This isn’t only for the scalp—a medicated shampoo can serve as a body wash in the shower to prevent breakouts.
Personal Hygiene: Showering promptly after sweating can greatly diminish the chances of developing fungal acne by keeping the skin clean and dry.
Tight, non-breathable clothing should be avoided since it can trap moisture and heat, fostering an environment where yeast thrives. Regularly changing bed linens can also help as it decreases the potential transfer of fungus to the skin.
Potential Complications
Fungal acne, if not treated properly, can lead to undesirable long-term effects. An awareness of these complications is critical in managing the condition effectively and minimizing its impact on skin health.
Long-Term Effects
Scarring: When fungal acne is severe or recurrent, it may cause permanent scarring on the skin. This is particularly true if the affected areas are subjected to manipulation, such as picking or scratching, which can exacerbate the inflammation and lead to tissue damage.
Recurrence: Even after treatment, fungal acne tends to recur, particularly in individuals with a predisposition to the condition or those living in warm, humid environments. Maintaining strict hygiene and a tailored skincare routine is essential in preventing relapses.
When to See a Dermatologist
When dealing with persistent breakouts that do not respond to over-the-counter treatments, it is important to consider consulting a dermatologist. They can provide a definitive diagnosis and tailored treatment plan.

Professional Advice
A board-certified dermatologist should be consulted when someone experiences a breakout that appears as uniform small pimples, particularly if these are accompanied by itching, and the condition persists despite general acne treatments.
Dermatologists are equipped to differentiate between fungal acne and other types of acne, such as bacterial, and recommend the appropriate course of treatment.
Although many skin conditions can be addressed with home remedies and over-the-counter products, a dermatologist’s intervention is often required for conditions that seem resistant or atypical.
They can determine whether the breakout is fungal and suggest treatment options, including antifungals and lifestyle modifications, that are customized to the patient’s unique skin concerns.
If there is any doubt, especially after a prolonged period of self-management without improvement, one should not hesitate to seek out professional advice. Early intervention by a dermatologist can prevent the worsening of the condition and lead to better long-term skin health.

